Each year since I started the blog, I have detailed my POTS and ME/CFS progress. This post is a continuation of that tradition.
A few things to consider:
- These changes happened very gradually and subtly over multiple years.
- This improvement has happened with the culmination of dozens of small things/treatments and time.
- I want to acknowledge that this is not indicative of everyone’s experience, so take this for what it is.
I developed POTS and ME in the spring/summer of 2017 and was diagnosed in August of 2018 (when it was its most severe for me). This compares my progress from 2018 to 2020-2022. To read about my path to diagnosis and journey with POTS and ME/CFS up until October of 2019, you can check out My POTS and ME Story.
Tilt testing
- 2018- My BP went hypertensive at the 1 minute mark and otherwise stayed normal. My heart rate jumped from 78 to 122 (increase of 44 bpm) and stayed in the POTS criteria range the whole time I was upright.
- 2020- Poor man’s tilt (so, this is not a scientific comparison). It’s important to note that I am currently taking Mestinon because it lowers the heart rate a bit. My BP drops about 20 points when I stand, but I don’t put a ton of stock in that because I’m just using an at-home machine. My pulse at laying down is 57 bpm. 30 seconds after standing it jumps to 107 bpm (a jump of 50 bpm). By the 1 minute mark, my heart rate is already back down to 75 and stays between there and the mid 80’s the whole ten minutes. According to my neurologist, I no longer meet POTS criteria because the heart rate increase must be sustained for a period of time.
- 2021- Based on how I feel, I am almost certain that I would continue to no longer meet POTS criteria. My heart rate monitor is on the fritz, so I did not retest this.
- 2022– I don’t have a heart rate monitor anymore, but I am guessing that I would still no longer meet POTS criteria.
Out of breath
- 2018- Very often.
- 2020- Occasionally.
- 2021- Rarely.
- 2022– Rarely.
“Gassed” feeling in muscles
- 2018- Severe, debilitating, and frequent. This is the sensation of the muscles having no oxygen and “burning”. The “burning” is not painful, it is a fatigue-inducing sensation. It is like having the feeling in the muscles like you just completed a 400m race… perpetually.
- 2020- This fluctuates. Most of the time it is mild, but sometimes it is more intense.
- 2021- This occurs pretty rarely and doesn’t bother me.
- 2022– I would say this is still pretty rare. However, I have been lifting more/heavier and having a greater overall activity level due to work and my muscles struggle sometimes. They feel like they don’t recover very well and get tight/junky feeling. For a while I considered this one in the same as “gassed” muscles, but I would characterize it as different upon more reflection.
Low grade fevers with fever symptoms
- 2018- Frequent.
- 2020- Fairly rare.
- 2021- No longer occurs.
- 2022– No longer occurs.
Sore throat
- 2018- Occasional.
- 2020- Rare.
- 2021- Extremely rare.
- 2022– No longer occurs.
Bloating
- 2018- Frequent and very significant.
- 2020- Sometimes it isn’t too bad, but for the most part it is still pretty frequent and significant.
- 2021- Same as last year.
- 2022– This and other GI issues got temporarily worse post-COVID, but now they are better than before.
Brain fog
- 2018- Major and debilitating. This was very upsetting and embarrassing in the beginning.
- 2020- I have a very minor brain mist as my husband lovingly says. Actually, it is rare that I notice this anymore. I feel very confident in my cognitive abilities.
- 2021- I still feel very confident in my cognitive abilities. I don’t have any consistent brain fog anymore. It only crops up in response to something like a random crash or overwhelm.
- 2022– My brain fog got worse for a few months after I got COVID-19, but now it’s back to only being an issue when I overdo it.
Driving ability
- 2018- Heck to the no.
- 2020- I can drive up to 30-45 minutes at a time on easy routes. Also, I drive like a grandma. I think this is more of a confidence issue now and I need more practice.
- 2021- I drive everywhere I need to go as normal. I don’t drive long-distance (ex. traveling out of state). I imagine that I could if I took breaks, but I don’t have the desire to try it at this point.
- 2022– I’m doing great with driving. I drive every day, sometimes up to an hour in one direction for work.
Pre-Syncope
- 2018- Frequent, and I would sometimes drop to the floor, but not fully faint. I like to call this maneuver the POTS, drop, and roll.
- 2020- This fluctuates. Sometimes, I will go a period of time without noticing it at all. Other times, I will notice it only when I crouch and then stand up. Occasionally, I will have a day/several days in a row where it’s like “WTH is going on!”. The good news is that my body regulates quickly and the sensation passes after a short period of time.
- 2021- This is a rare occurrence.
- 2022– This has been happening more frequently this year, but it still passes through quickly, so I’ve been fine. For example, I’ll squat down, stand up, see stars and hold on to something, then I’m fine several seconds later.
Fatigue
- 2018- Severe, debilitating, and constant. I was functioning around 30% of normal. I could do a little beyond taking care of my basic needs.
- 2020- This is still my most limiting factor, but this has improved significantly. I function around 70% of normal now and feel better. When I speak in percentages like that, 100% would be able to function like my peers, not necessarily feeling perfectly amazing. I do not consistently feel 70%. It will dip sometimes. But, for the most part, I can stay functioning at that 70% without “paying for it” despite a dip in how I feel.
- 2021- I function around 80% of normal most of the time, which is amazing. Energy improvement has come subtly and slowly, but I can see the change when I compare what I can do in a day now compared to last year.
- 2022– I function around 85% of normal most of the time and during the daytime. I have continued to see gradual improvement. Evenings are a little harder for me now, though, because the Post-COVID booster pain catches up to me and I get more fatigued than I used to during that time.
Energy crashes/Post-exertional malaise
- 2018- Frequent and they would take several days to bounce back from.
- 2020- Occasional and they take less than a day to bounce back from.
- 2021- Rare and still take less than a day to bounce back from.
- 2022– Same as last year.
Cycles
- 2018- Menorrhagia, oligomenorrhea.
- 2020- I alternated between what is listed above and normal early in the year, but the last few cycles have been normal.
- 2021- Normal.
- 2022– Normal.
Noise/commotion sensitivity
- 2018- Sensitive to always.
- 2020- This only bothers me if I am in a crash and it is still less bothersome at that.
- 2021- Same as last year.
- 2022– Same as last year.
Muscle weakness
- 2018- Useless noodle body. My hip flexors were especially weak- this happened at the onset of the illness. I became so weak in the year before I was diagnosed that my husband would have to carry me up the stairs.
- 2020- I am much stronger and feel like an athlete again. My hip flexors still struggle despite me working on this consistently, though.
- 2021- I continue to get stronger and have more stamina as time goes on.
- 2022– Continued gains.
Vestibular ocular reflex issues
- 2018- My vision was “off” in a way that is hard to explain. I used to explain it like a drunk feeling, but not exactly like that. Another way to explain is like in That 70’s Show when Eric would talk to his parents after he came up from the basement and the walls would swirl behind them, but to a much lesser degree.
- 2020- I do not notice this at all anymore. Three cheers for physical therapy!
- 2021- No issues.
- 2022– No issues.
Heat and cold intolerance
- 2018- Basically like a cold-blooded lizard.
- 2020- I kicked butt with the heat this summer. I am not cold intolerant, but I still despise it. My google searches for “warm places to live” have gone up exponentially this month.
- 2021- I continue to tolerate the heat and the cold better as time goes on.
- 2022– I think I’m normal in this regard now.
Acute illness and sinus infections
- 2018- Every time I would get sick (which was constantly), it would turn into a sinus infection.
- 2020- I haven’t gotten a sinus infection in about 10 months. I also have only gotten sick once in that time period. I believe COVID-19 measures are the largest factor in this.
- 2021- I’ve stayed healthy and have had zero sinus infections.
- 2022– I’ve been healthy except for a bout of COVID-19 in February of this year.
Blood pooling
- 2018- I would occasionally notice where my feet would have the blood pooling in them. Or, I would lay with my legs up and my feet and lower legs would go white.
- 2020- I can’t remember the last time I noticed this.
- 2021- Same as last year.
- 2022– Same as last year.
Cold hands and feet
- 2018- Ice, ice, baby.
- 2020- Vanilla ice, ice baby. Too cold, too cold. They are my secret weapon when my husband is looking a little too comfortable.
- 2021- I notice it in the winter, but I don’t think it’s a problem.
- 2022– Normal and random.
Exercise tolerance
- 2018- I could tolerate 3 minutes of slow, easy movement.
- 2020- I exercise for 30-60 minutes every day doing: yoga, walking, dance cardio, and HIIT workouts.
- 2021- I exercise for almost two hours every day doing: weight lifting, walking, running, drills, and stretching. I have better non-exercise movement tolerance as well.
- 2022– I exercise around an hour each day doing similar activities to last year. Although I exercise less, I work more and my jobs are physical.
Dry eyes
- 2018- No problems.
- 2019- Dry eye syndrome and blepharitis.
- 2020- Prone to the issues above, but it’s under control/treated.
- 2021- I’m still prone to those issues and they occasionally become a nuisance, but it’s mostly under control.
- 2022– This has been a little more annoying this year, but it’s still mostly under control.
Headache
- 2018- I used to get a sensation of pressure around the base of my head. It was a different than a headache, but I don’t know what to call it.
- 2020- I do not notice this anymore.
- 2021- Not an issue.
- 2022– For most of 2022, none. However, I get headaches now due to the COVID-19 booster reaction. They occur a couple times per week, mostly in the evening or when I get worn out. This is improving gradually over time.
Pain
- 2018– Occasional mild fever body ache sensation during crashes.
- 2020– Rare body aches.
- 2021– Very rare body aches.
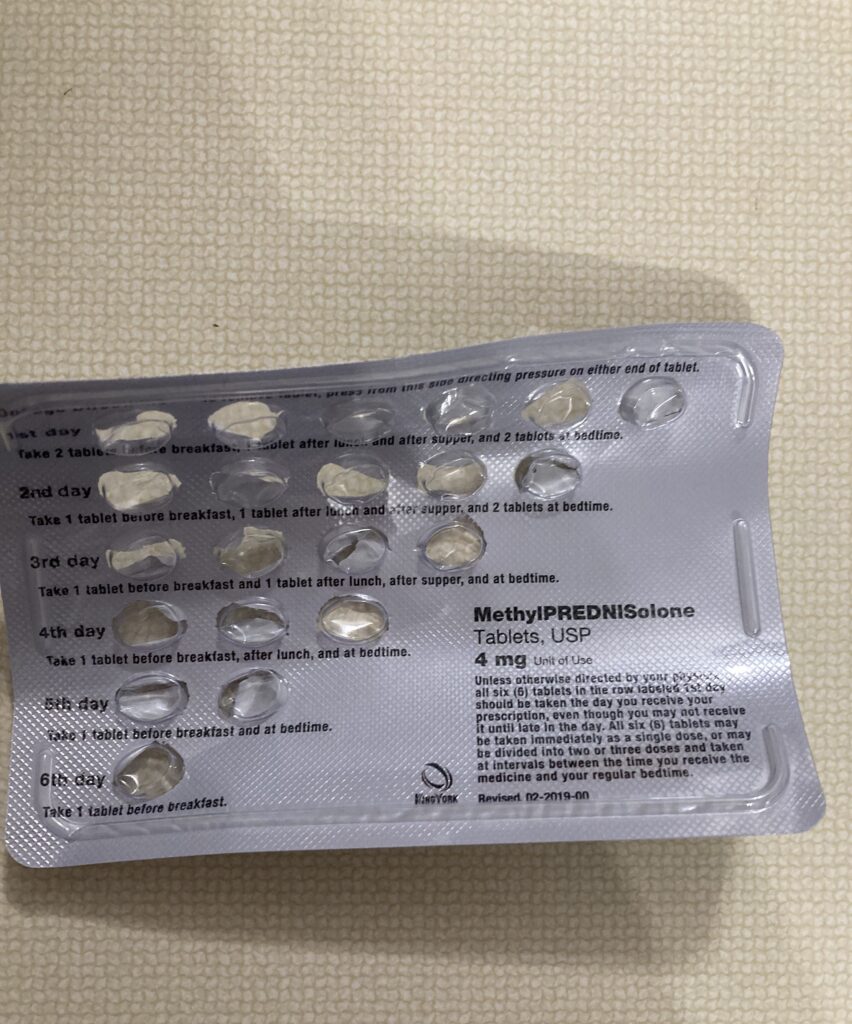
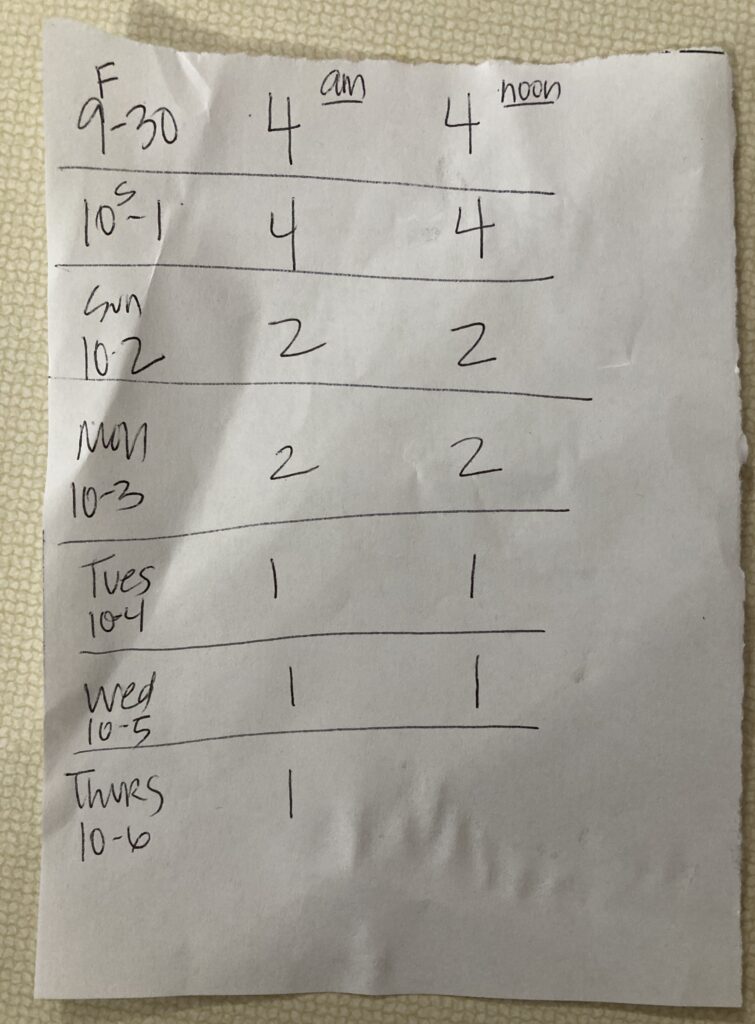
- 2022– Very rare for most of the year. However, since the booster I get frequent, mild body aches that span from my head, down my neck, and down my arms into my hands. The pain has definitely improved after two courses of prednisone and with time.
Heart Arrythmias
- 2018– None.
- 2020– None.
- 2021– None.
- 2022– After the COVID-19 infection in February, I had PVCs for around three months. Then, I was fine until I received the COVID-19 booster in the fall. Now, it feels like I get something. Perhaps it’s just more tachycardia than I’m used to. It’s hard to put my finger on what it is, but it feels like a random flutter in my chest. I haven’t gotten it evaluated yet because I don’t think it coincides with any other symptoms.
Sleep
- 2018- Rare insomnia.
- 2020- No sleep problems.
- 2021- No issues.
- 2022– No issues.
This past year has been a bit of a mixed bag. Overall POTS and ME/CFS-wise, I think I have had some encouraging improvement. My overall quality of life is better. However, I have had some struggles due to COVID and the booster. The COVID struggles are over and I am optimistic that the new issues that cropped up from the booster will eventually subside.
How has your POTS or ME/CFS progressed over the years?
Disclaimer: I am not a medical professional. Statements on this site are not meant to be taken as medical advice. These statements reflect my personal experiences having mild-ish post-viral POTS and ME. Due to the wide spectrum of these diseases, comorbidities, and everyone being different, your experiences may be very different than mine.
Note: If you post a comment, this site does NOT have a feature to notify you of responses to your comment. I have not found a good solution for that yet. However, I usually respond to every comment in a timely manner, so be sure to check back.